The demand for cognitive health services within the U.S. healthcare system is steadily increasing. To illustrate, 1 in 9 adults aged 65 and above suffer from Alzheimer’s disease (AD), with over 60% of dementia cases going undiagnosed. Early diagnosis of Mild Cognitive Impairment (MCI) and dementia is important because it leads to diagnosing and treating the underlying cause earlier. The increasing need for early detection and treatment of MCI and AD, coupled with the pressing necessity to identify high-risk patients, underscores the pivotal role of digital cognitive health solutions in the hands of PCPs.
These tools empower PCPs to swiftly, accurately, and easily detect these diseases at their earliest stages, facilitating timely referrals to specialist physicians for those in need. Moreover, digital tools require less time and resources, streamlining the diagnostic process and enhancing overall efficiency.
Why is the Need for Early Detection of MCI/AD Conditions Imperative?
According to the Alzheimer’s Association, approximately 12% to 18% of people aged 60 or older are living with MCI. An estimated 10% to 15% of individuals living with MCI develop dementia each year. Many cases of MCI are reversible. Now it is possible to delay cognitive disease progression with new therapeutics and there are more effective treatments in the early stages.
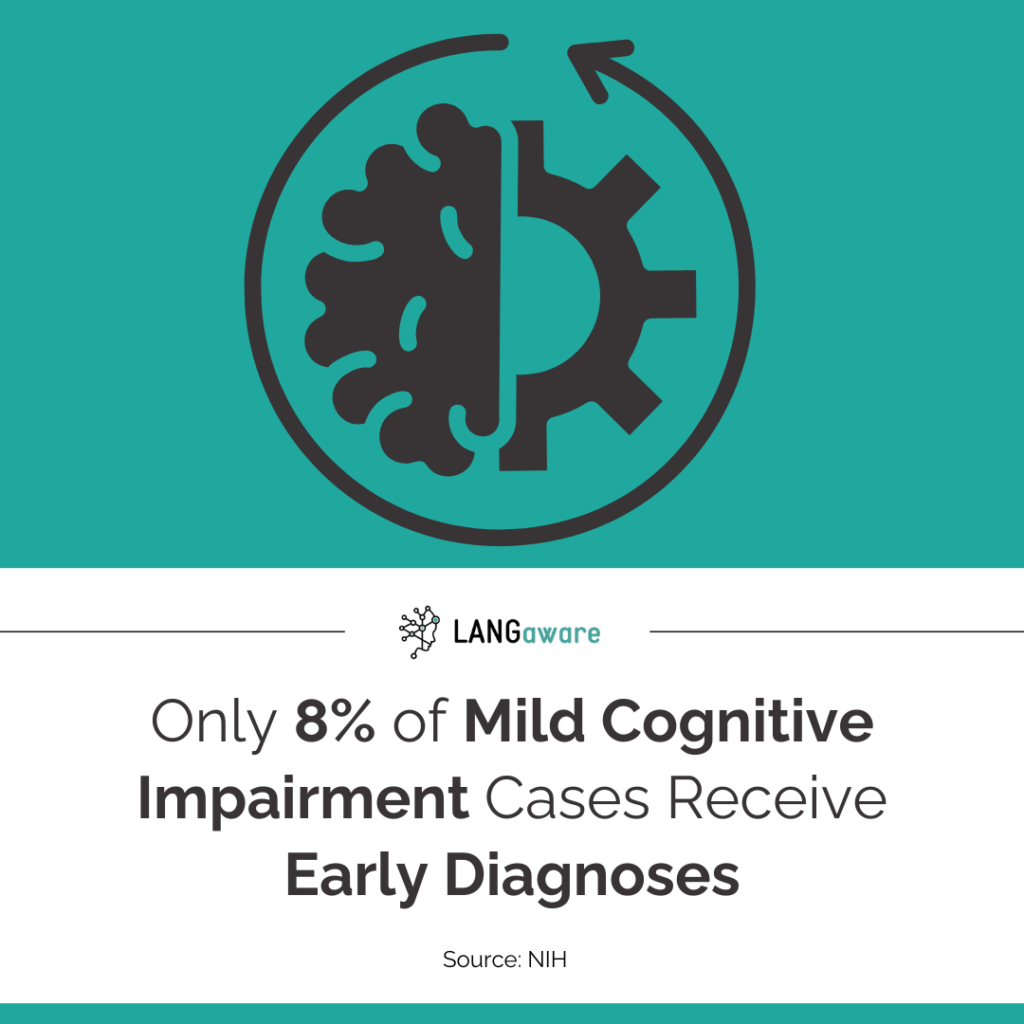
Traditional healthcare systems face several limitations in meeting this demand, including lack of resources and lack of access. According to STAT, critical to the race for early diagnosis and treatment of AD is unexpectedly the primary care provider (PCP). According to the Alzheimer’s Association, about 85% of people diagnosed with some form of dementia first receive that diagnosis from a non-dementia specialist, typically a PCP. However, there is a shortage of PCPs in the U.S. and many PCPs don’t feel comfortable assessing cognition. This unease likely stems from a lack of training, time, and uncertainty about diagnosis and treatment. According to NIH, MCI is vastly underdiagnosed, pointing to an urgent need to improve early detection in primary care: only about 8% of expected cases were diagnosed on average.
What are the Benefits of Digital Cognitive Health Solutions for Health Systems?
According to the U.S. Government Accountability Office, there are several machine learning (ML) technologies available in the U.S. to assist with the diagnostic process. The resulting benefits include earlier detection of diseases; more consistent analysis of medical data; and increased access to care, particularly for underserved populations. These innovations could enhance medical professionals’ capabilities and improve patient treatments as they can be used to monitor disease progression and treatment efficacy.
Digital tools for cognitive health diagnosis can be self-administered, thus enabling remote diagnosis, while also requiring fewer resources since they do not necessarily need a clinician to administer them. These tools optimize the diagnostic process by making it easier, faster, more objective, and accurate. They can aid PCPs in decision-making regarding MCI and AD diagnosis, thereby expediting referrals to specialists. Furthermore, digital tools can promote inclusivity and improve access for all individuals, leading to better patient outcomes and engagement, as well as reduced costs and hospital overflow.
As Alzheimer’s Research & Therapy points out, in an era of growing patient numbers, digital cognitive testing holds considerable value because it allows for cost-effective testing through self-administration and can serve several purposes: as a screening tool, monitor disease progression during follow-up visits after diagnosis, and to measure treatment response.
Types of Digital Cognitive Health Solutions
According to NIH remote and in‐clinic digital cognitive screening tools outperform the MoCA to distinguish cerebral amyloid status among cognitively healthy older adults. More specifically, in recent years, there has been significant progress in the development of tablet-based cognitive assessments, proving their accuracy and reliability for both in-person and remote administration. These assessments offer greater flexibility in accommodating diverse ethnicities, cultures, and languages. Similarly, smartphone apps and web-based cognitive assessments have emerged as effective tools for remote screening and monitoring, capitalizing on the increasing use of smartphones and tablets among older adults.
The adoption of digital cognitive assessments in remote and primary care settings offers various benefits, including reducing the burden on practitioners, facilitating repeat testing, and improving the cost-effectiveness and efficiency of care delivery. Moreover, digital assessments have the potential to bridge gaps in healthcare access by reaching underserved populations and adapting to different languages, thereby promoting inclusivity and addressing healthcare disparities.
As Bertalan Meskó points out in his analysis of the future of cognitive health and how digital health can help, there are several alternatives such as dedicated AI algorithms, cognitive training apps, machine learning for early detection to name a few.
With record levels of older adults currently living with AD, there is an urgent need for more sensitive and scalable screening tools to facilitate earlier diagnosis and intervention for AD and related dementias. Access to digital tools that facilitate this, like LANGaware’s screening and monitoring tool, can prove invaluable to contain a problem that is already big.
Addressing Challenges and Concerns with Digital Cognitive Health Solutions
There are several challenges and concerns related to digital solutions, these issues include a) security and confidentiality; b) safety and ease of use; c) the need for a strong data infrastructure and back-up expertise; d) easy integration e) easy sharing of data; f) value proposition for everyone on the table; g) scalability; h) patient engagement and outcomes.
Addressing these challenges in digital cognitive tools requires a comprehensive approach.
First, robust security measures must be implemented to ensure privacy and confidentiality of patient data. Safety and ease of use are crucial considerations, requiring user-friendly interfaces and clear instructions.
A strong data infrastructure and expertise are essential for managing and safeguarding data effectively. Integration with existing healthcare systems should be seamless to encourage adoption and facilitate data sharing among different providers. The value proposition of digital tools must be clearly demonstrated to stakeholders, highlighting the benefits for patients, healthcare professionals, and organizations.
Scalability is another important factor, as digital tools should be able to accommodate growing user bases and evolving healthcare needs. Patient engagement strategies should be employed to promote active participation and improve outcomes. Overall, addressing these challenges involves a combination of technological innovation, regulatory compliance, and user-centered design principles.
Embracing Digital Cognitive Health Solutions
As NIH points out, with record levels of older adults currently living with Alzheimer’s disease, there is an urgent need for more sensitive and scalable screening tools to facilitate earlier diagnosis and intervention for Alzheimer’s disease and related dementias. An estimated 95 million Americans —one-quarter of the population — will be 65 or older by 2050, and nearly 14 million people will have Alzheimer’s.
With a rapidly aging population, there’s a pressing need for more sensitive and scalable screening tools to enable earlier diagnosis and intervention. However, the current healthcare landscape faces significant challenges in this regard. Despite mandates for cognitive assessments in primary care settings, cognitive impairment often goes unrecognized or misdiagnosed, partly due to limitations in existing screening tools and PCPs discomfort with assessing cognition. Moreover, the burden on primary care is compounded by the broader challenges facing healthcare systems worldwide, including aging populations, rising complexity, and personnel shortages.
Looking Ahead
Embracing technology in healthcare offers a promising avenue to alleviate some of the challenges mentioned. By leveraging innovative solutions, such as digital cognitive health screening tools, healthcare providers can streamline workflows, prevent burnout, and enhance patient care. As the number of people with dementia is expected to double by 2050, timely and accurate diagnosis becomes increasingly critical.